What do diabetes, arteries and peripheral arterial disease have in common? People with diabetes who have uncontrolled blood sugars for a long time are at high risk of developing blood vessel damage and peripheral artery disease (PAD). However, not every person with diabetes develops PAD. Results from the Framingham Heart Study show that up to 20%-30% of people with PAD have diabetes.1 That said, people with a less severe form of PAD may not have any symptoms, or people with more severe PAD have altered pain perception due to nerve damage and remain undiagnosed. Hence, this figure fails to represent the actual number of people with diabetes who develop PAD.
In people with diabetes, peripheral arterial disease (PAD) usually affects arteries below the knees and is severe enough to cause amputation of the affected area. The amputation rates in diabetic people with PAD are higher than those without diabetes, with rates ranging from 5 to 15 times greater according to a few studies.2 Knowing how diabetes leads to PAD is thus of utmost importance to help you make an informed decision and take steps to prevent PAD beforehand.
How Does Diabetes Trigger PAD?
A buildup of fatty plaque (Atherosclerosis)
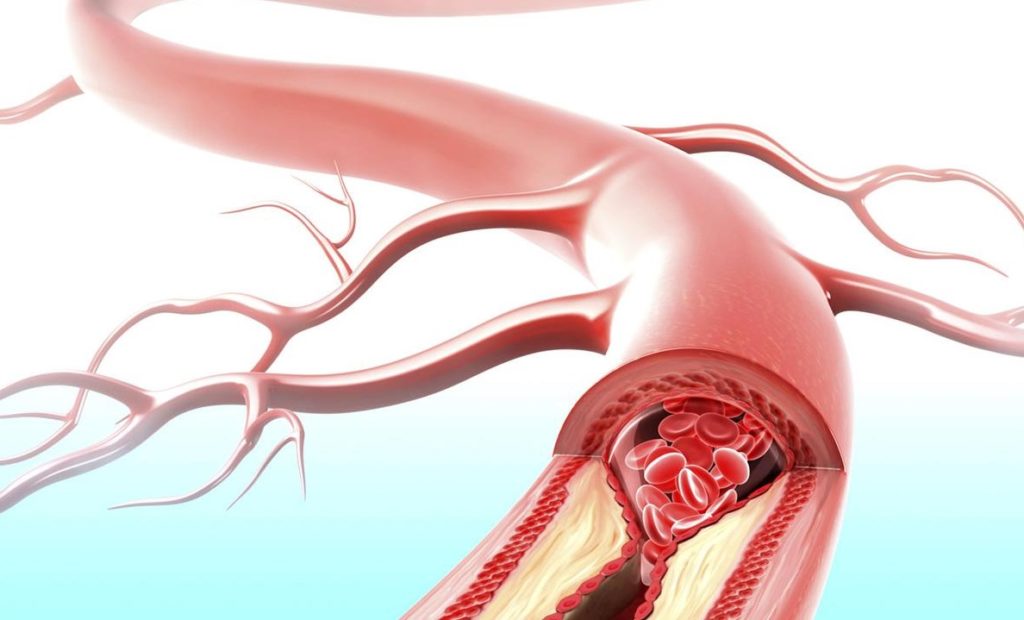
The key mechanism through which diabetes leads to PAD is a buildup of a waxy substance called fatty plaque (fatty deposit) inside the arteries supplying blood to your limbs. Scientifically known as atherosclerosis, this process hardens and narrows your arteries, slowing down the blood flow. Even worse, the high blood sugars raise the levels of certain inflammatory substances in your blood that trigger blood clots if the plaque breaks open, completely cutting off the blood supply. Normally, the blood clot forms to prevent bleeding. But it can also develop where it’s not needed, such as in your blood vessels.2 As a result, the arteries can no longer carry oxygen-rich blood to your limbs, primarily the legs, which experience the hallmark “walking-calf pain (known as intermittent claudication)” of PAD.
This same mechanism provokes heart attacks and stroke, which is why diabetes can end up in these complications too.
Reduced nitric oxide production
In diabetes, various factors suppress the release of nitric oxide—a chemical that normally works to dilate (aka widen) your blood vessels, such as:
Damage to the endothelium
Long-standing low-grade inflammation stemming from diabetes damages the inner lining of your blood vessels called endothelium. This endothelium is responsible for the release of nitric oxide. Hence, damage to the endothelium impairs the release of this compound. The affected blood vessels have a hard time opening up, slowing the blood flow through them.2
Insulin resistance
In healthy people, the blood sugar-lowering hormone, insulin helps with the production of nitric oxide that keeps the blood vessels patent. However, in people with diabetes, the insulin resistance interferes with nitric oxide production, which in turn, restricts the blood flow through the blood vessels, including those delivering blood to the legs.3
Advanced Glycation End Products (AGEs)
AGEs are harmful products formed when protein or fat mixes with the sugar in your bloodstream. Being a distinctive feature of diabetes, the AGEs produce free radicals and plenty of inflammatory substances that induce widespread damage. These compounds recruit the white blood cells to the site of injury and then transform them into fat-laden cells with a foamy appearance (these foam cells serve as the earliest hallmark of the fatty plaque).4,5 To make things worse, the AGEs also block nitric oxide production, all in all, leading to the arterial damage seen in PAD.5

How Is Peripheral Arterial Disease Treated?
If you do not have any symptoms of Peripheral Arterial Disease (PAD), you are likely to benefit from preventive strategies, such as strict control of blood sugars and weight. Supervised exercise programs not only help with leg pain and walking endurance, but also aid in controlling weight that could otherwise destabilize your blood sugars.
Individuals with symptomatic PAD are treated with blood thinners and cholesterol-lowering medications called statins to reduce their risk of amputation as well as a preventive strategy of dying from heart attacks and strokes. Another medication called cilostazol helps speed up the blood flow to the limbs and address symptoms of claudication both by keeping the blood thin and by expanding the blood vessels.
Some people with PAD, will however, continue to experience limited walking ability and a reduced quality of life. If the symptoms fail to respond to medical treatment, your vascular specialist will recommend peripheral artery angioplasty and stenting to open up the blocked arteries and restore blood flow to your legs.
Peripheral Angioplasty
Angioplasty is a procedure carried out in the operating room/catheterization) lab. You’ll be lying down on a table under sedation to help you relax. Guided by an x-ray image on a monitor, a thin flexible tube called a catheter is then advanced through the arteries to the site of blockage.
The tip of the catheter has a small balloon attached to it that is inflated to reopen the narrowed segment of the artery and restore the blood flow. The balloon is then deflated and removed.
Stent Placement
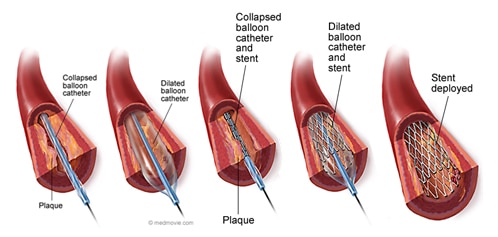
In some cases, your doctor will also place a metal tube that has a mesh framework called a stent to prop the artery open and reduce the chances of the artery narrowing again. Once the stent is in its place, your doctor will remove all the tubes.
The likelihood that the treated vessel will remain patent following angioplasty is 81.6% at 3 years.6 You’ll be put on blood thinners after restoring the blood flow to prevent re-blockage.
Schedule an Appointment to Learn More
At Precision Vascular, we incorporate some of the most cutting edge technologies in treating Peripheral Arterial Disease such as atherectomy, intravascular ultrasound and drug-eluting technology. Call us at 214-382-3200 to schedule a consultation or complete the form below.
Precision VIR serves the DFW area including Dallas, Fort Worth, Carrollton, Richardson, Garland, Mesquite, Highland Park, University Park, Park Cities, Allen, Plano, Frisco, McKinney, Arlington, Irving, Grand Prairie, Farmers Branch, Denton, Lewisville and all of North Texas.
This information is not a substitute for professional medical advice. Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider.
Sources
- Murabito JM, D’Agostino RB, Silbershatz H, Wilson WF. Intermittent claudication. A risk profile from The Framingham Heart Study. Circulation. 1997;96(1):44-9.
- Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes. 2015;6(7):961-9.
- Moore KJ, Sheedy FJ, Fisher EA. Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol. 2013;13(10):709-21.
- Armstrong EJ, Rutledge JC, Rogers JH. Coronary artery revascularization in patients with diabetes mellitus. Circulation. 2013;128(15):1675-85.
- Muniyappa R, Sowers JR. Role of insulin resistance in endothelial dysfunction. Rev Endocr Metab Disord. 2013;14(1):5-12.
- Morris-Stiff G, Moawad M, Appleton N, et al. Long-term clinical outcome following lower limb arterial angioplasty. Ann R Coll Surg Engl. 2011;93(3):250-4