Peripheral Arterial Disease (PAD) – Definition
Peripheral Arterial Disease or Peripheral Artery Disease (PAD), also referred to as arteriosclerosis of the extremities and peripheral vascular disease, is a condition that causes poor blood circulation to the kidneys, intestines, arms, legs, and feet. Blood flow may be reduced or blocked by narrowed or hardened blood vessels. This can lead to tissue and nerve injury or damage. You may decrease your risk of PAD by reducing the risk factors that you can control. PAD is treated with medications and surgery. In severe cases, amputation may be necessary.
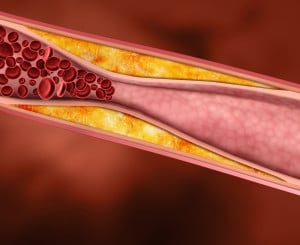
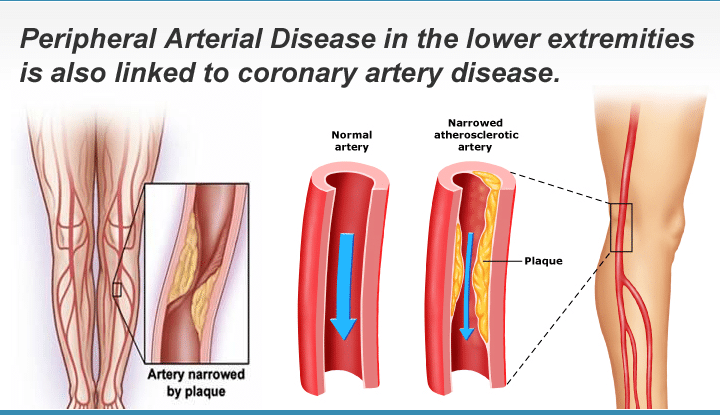
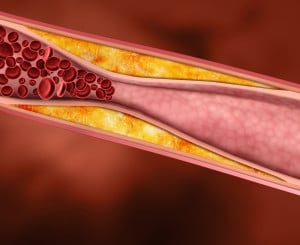 PAD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries. This is a very serious condition. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking, and eventually gangrene and amputation.
PAD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries. This is a very serious condition. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking, and eventually gangrene and amputation.
Because atherosclerosis is a systemic disease (that is, affects the body as a whole), individuals with PAD are likely to have blocked arteries in other areas of the body. Thus, those with PAD are at increased risk for heart disease, aortic aneurysms and stroke. PAD is also a marker for diabetes, hypertension and other conditions.
PAD may also be caused by blood clots.
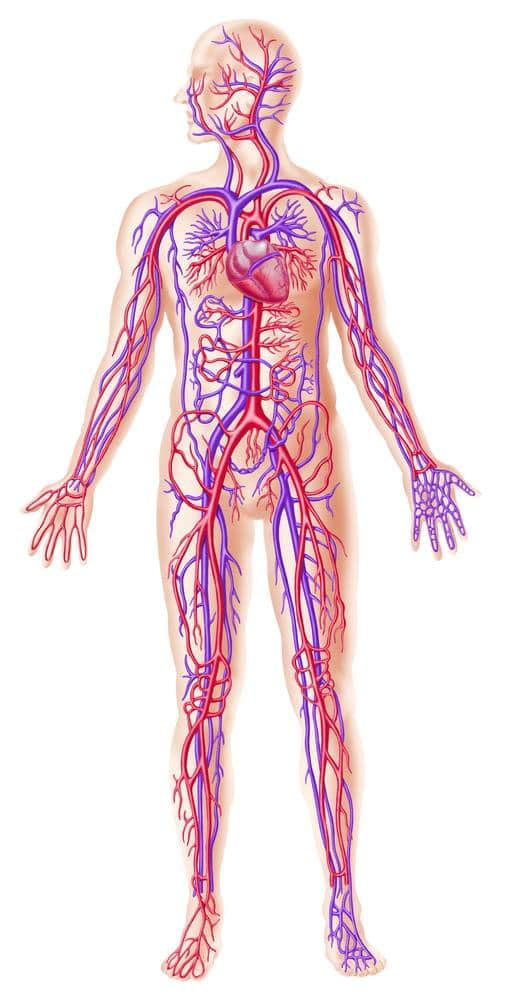
Anatomy
The heart has several large arteries and veins connected to it that branch out and become smaller as they travel throughout your body. Your arteries and veins are blood vessels that deliver blood throughout your body in a process called circulation. Arteries carry oxygenated blood away from your heart. Veins carry deoxygenated blood from your body and lungs back to your heart.
Causes
 PAD results when the arteries that supply the kidneys, intestines, arms, legs, or feet become narrow and hard. Hardening of the arteries usually develops first in the legs and feet. The arteries become less elastic, narrow, and hard because of calcium deposits on the wall of the artery. The artery may completely close, preventing blood flow. The artery may be unable to dilate (become larger) to carry more blood especially during periods of exercise. The lack of blood flow can contribute to nerve and tissue injury and damage.
PAD results when the arteries that supply the kidneys, intestines, arms, legs, or feet become narrow and hard. Hardening of the arteries usually develops first in the legs and feet. The arteries become less elastic, narrow, and hard because of calcium deposits on the wall of the artery. The artery may completely close, preventing blood flow. The artery may be unable to dilate (become larger) to carry more blood especially during periods of exercise. The lack of blood flow can contribute to nerve and tissue injury and damage.
Symptoms
The early symptoms of PAD usually begin in the legs and feet. It may affect one leg or both legs to different extents. The symptoms of PAD are often mistaken for something else.
- The most common symptom of PAD is called intermittent claudication, which is painful cramping in the leg or hip that occurs when walking or exercising and typically disappears when the person stops the activity.
- Numbness, tingling and weakness in the lower legs and feet and appear pale or blue.
- Difficulty walking
- Burning or aching pain in feet or toes when resting
- Sore on leg or foot that won’t heal
- Cold legs or feet
- Color change in skin of legs or feet
- Loss of hair on legs
- Pain in the legs or feet that awakens you at night
- Pulse in the affected limb may be weak or absent.
Many people simply live with their pain, assuming it is a normal part of aging, rather than reporting it to their doctor.
Peripheral Arterial Disease Treatment
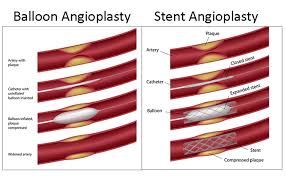
PAD is treated with medications and surgery. The purpose of treatment is to relieve symptoms and improve circulation. Medications may be used to thin the blood and open the arteries to increase blood flow. Surgery may be used to repair the lining of an artery, replace the affected artery with a graft, or bypass the affected area with a synthetic blood vessel or a vein. Balloon angioplasty, stents, and laser treatments may help as well.
Angioplasty and stenting
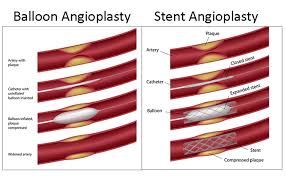
Interventional radiologists pioneered angioplasty and stenting, which was first performed to treat artery disease. Using imaging for guidance, the interventional radiologist threads a catheter through the femoral artery in the groin, to the blocked artery in the legs. Then the interventional radiologist inflates a balloon to open the blood vessel where it is narrowed or blocked. In some cases, this is then held open with a stent, a tiny metal cylinder. This is a minimally invasive treatment that does not require surgery, just a nick in the skin the size of a pencil tip. Balloon angioplasty and stenting have generally replaced invasive surgery as the first-line treatment for Peripheral Arterial Disease (PAD). Early randomized trials have shown interventional therapy to be as effective as surgery for many arterial occlusions, and in the past years, a very large clinical experience in centers throughout the world has shown that stenting and angioplasty are preferred as a first-line treatment for more and more processes throughout the body.
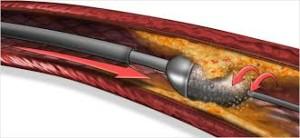
Atherectomy
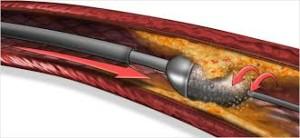
With this treatment, a tiny catheter is inserted into the artery at the site of blockage that is able to “shave” or “cut” the plaque from the inside of the artery and remove it from the patient.
Stent-grafts

A stent covered with synthetic fabric is inserted into the blood vessels to bypass diseased arteries.
Surgery

Sometimes, open surgery is required to remove blockages from arteries or to bypass the clogged area. These procedures are performed by vascular surgeons.
 Peripheral Arterial Disease Prevention
Peripheral Arterial Disease Prevention
You may prevent PAD by reducing the risk factors that you have control over including your weight, blood pressure, diabetes, cholesterol, and activity level. You should quit smoking. It can be helpful to exercise regularly and eat a well-balanced diet. You should make and attend all of your doctor appointments.
Am I at Risk?
People with all of the risk factors may never develop PAD; however, the chance of developing the condition increases with the more risk factors you have. You should tell your doctor about your risk factors and discuss your concerns.
Is Treatment for PAD Right For You?
Wondering if treatment for Peripheral Arterial Disease is right for you? Download our FREE PAD Check List to help you decide!

Complications
PAD may lead to foot or leg infection, sores, or ulcers. In some cases, especially among people with diabetes, amputation may eventually be necessary. PAD can lead to impotence. PAD can cause dangerous embolisms, blood clots that travel in the bloodstream.
F.A.Q.
What Increases My Risk of PAD?
Many things can increase your risk for atherosclerosis and peripheral arterial disease (PAD). These include:
- Smoking.
- High cholesterol.
- High blood pressure.
- Diabetes. People with diabetes often have arterial disease that is both more severe and more widespread than in people who don’t have diabetes.
- A family history of atherosclerosis or coronary artery disease.
The risk for Peripheral Arterial Disease (PAD) also increases with age.
People who have the disease in one part of the body are likely to have it in other places, including the legs.
Are My PAD Symptoms An Emergency?
Call us immediately if you suddenly have severe leg pain; numbness; or pale, blue-black skin.
Call your doctor if you have:
- Leg pain that begins after you walk a certain distance and that goes away when you rest (intermittent claudication).
- Foot or toe pain when you are resting.
What Lifestyle Changes Can I Make To Improve My PAD Symptoms?
- Quit smoking and avoid secondhand smoke. Smoking is a major risk factor for peripheral arterial disease. Quitting smoking may help prevent PAD or slow its progression. For more information on how to stop smoking, see the topic Quitting Smoking.
- Get regular exercise (if your doctor says it’s safe). Try walking, swimming, or biking for at least 30 minutes on most, if not all, days of the week. If you have intermittent claudication when you exercise, your doctor might recommend a walking program that might relieve your symptoms.
- Stay at a healthy weight.
- Eat heart-healthy foods, such as fruits and vegetables.
- If you have diabetes, keep your blood sugar in your target range.
- Avoid getting sick from the flu. Get a flu shot every year.
A cardiac rehab program can help you make lifestyle changes. In cardiac rehab, a team of health professionals provides education and support to help you make new, healthy habits.
Care for your feet and legs
Take good care of your feet and legs. When you have reduced bloodflow to your legs, even minor injuries can lead to serious infections.
- Treat wounds, cuts, and scrapes on your legs right away. Poor bloodflow to the legs caused by PAD can keep wounds, cuts, and scrapes from healing properly. Prompt treatment can help you avoid this problem and is especially important for people who also have diabetes.
- Avoid shoes that are too tight or that rub your feet. Shoes should be comfortable and fit well. Avoid socks or stockings that are tight enough to leave elastic-band marks on your legs. They can make circulation problems and symptoms from PAD worse.
- Keep your feet clean and moisturized to prevent your skin from drying and cracking. Place cotton or lamb’s wool between your toes to prevent rubbing and to absorb moisture.
- If open sores form, keep them dry and cover them with nonstick bandages. See your doctor as soon as you discover an open sore.
 PAD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries. This is a very serious condition. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking, and eventually gangrene and amputation.
PAD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries. This is a very serious condition. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking, and eventually gangrene and amputation.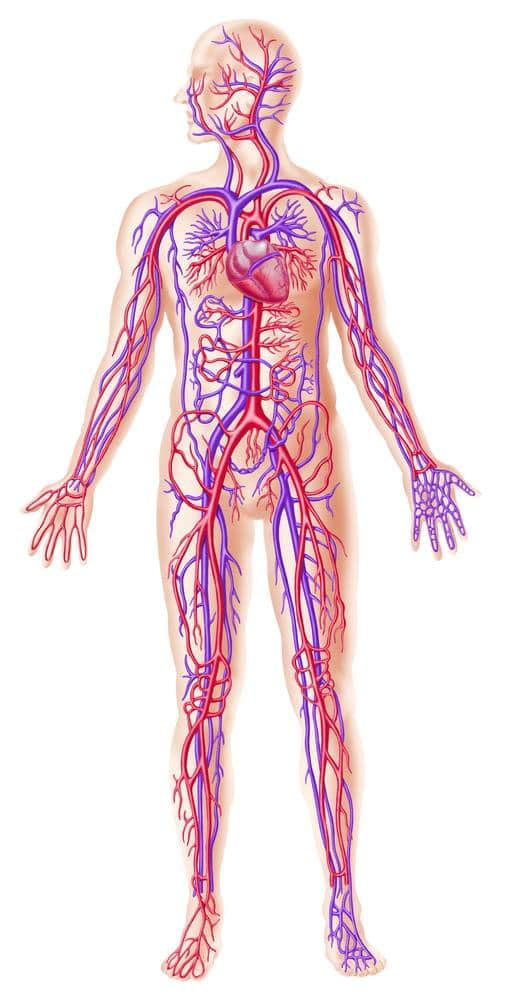
 PAD results when the arteries that supply the kidneys, intestines, arms, legs, or feet become narrow and hard. Hardening of the arteries usually develops first in the legs and feet. The arteries become less elastic, narrow, and hard because of calcium deposits on the wall of the artery. The artery may completely close, preventing blood flow. The artery may be unable to dilate (become larger) to carry more blood especially during periods of exercise. The lack of blood flow can contribute to nerve and tissue injury and damage.
PAD results when the arteries that supply the kidneys, intestines, arms, legs, or feet become narrow and hard. Hardening of the arteries usually develops first in the legs and feet. The arteries become less elastic, narrow, and hard because of calcium deposits on the wall of the artery. The artery may completely close, preventing blood flow. The artery may be unable to dilate (become larger) to carry more blood especially during periods of exercise. The lack of blood flow can contribute to nerve and tissue injury and damage. Peripheral Arterial Disease Prevention
Peripheral Arterial Disease Prevention


 Sometimes, open surgery is required to remove blockages from arteries or to bypass the clogged area. These procedures are performed by vascular surgeons.
Sometimes, open surgery is required to remove blockages from arteries or to bypass the clogged area. These procedures are performed by vascular surgeons.